
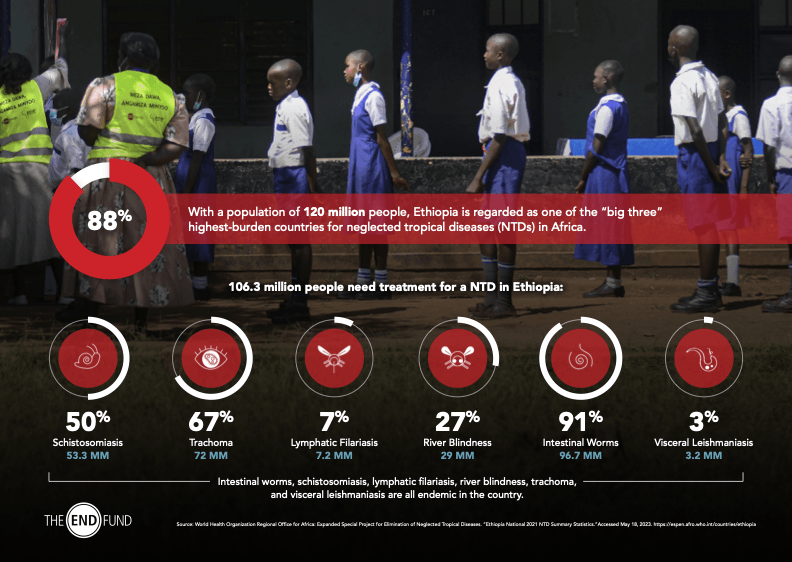
Students receive treatment during a school-based mass drug administration for intestinal worms and schistosomiasis in Amhara Region, Ethiopia.
The Ten Year Journey of
Ending NTDs in Ethiopia
The END Fund began working in Ethiopia in 2013, a collaboration that has now seen ten years of partnership towards ending NTDs in the country.
When the Ethiopian Federal Ministry of Health (FMoH) launched its NTD Master Plan in July 2013, they prioritized efforts to tackle schistosomiasis and intestinal worms. With this mandate, in 2014 the END Fund began to work with the FMoH, in collaboration with other partners, to provide deworming treatments to nearly eight million children in the first year alone.
In 2015, the END Fund joined a consortium of partners to support the FMoH in developing and implementing an ambitious five-year national deworming program to scale treatment to all school-age children at risk of schistosomiasis and soil-transmitted helminths (STH). Through this five-year initiative, the FMoH scaled up to reach over twenty million children at risk.
Over the years, the END Fund has broadened its support to Ethiopia’s NTD efforts outside of deworming by funding strategic initiatives for trachoma, river blindness, VL and LF as well.
With more than seventy-seven million people in need of treatment, Ethiopia is regarded as one of the “big three” highest-burden countries for NTDs in Africa along with the Democratic Republic of Congo and Nigeria. Intestinal worms, schistosomiasis, LF, onchocerciasis, and trachoma are all endemic in the country.
All four of the END Fund’s programmatic investment portfolios are active in Ethiopia. Since 2017, RLMF-supported areas in Ethiopia have seen remarkable progress in eliminating LF as a public health problem. Two districts near Sudan have passed two successive transmission assessment surveys (TAS), and two more zones bordering South Sudan have also passed their first TAS. TAS is a process used to determine if an area no longer has active transmission of a disease and, therefore, can stop conducting MDAs.
In September 2018, the Helmsley Charitable Trust invested through the END Fund’s Flagship Fund to support Ethiopia’s goal of eliminating trachoma by providing more than 95,000 trachomatous trichiasis (TT) surgeries by the end of 2023.
Through this support, TT surgical services became available in the Afar, Benishangul-Gumuz, Gambella, and Somali regions for the first time. In addition to surgeries, the END Fund partnered with the University of North Carolina to increase the number of certified national master TT surgery trainers in the country. These efforts are instrumental in strengthening the health system and supporting Ethiopia’s efforts to continue providing these essential health services.
Additionally, through the DIF, launched in April 2019, the END Fund aimed to accelerate progress toward the interruption of transmission of intestinal worms and schistosomiasis in Ethiopia.
With improved mapping, the FMoH will be able to target more specific areas and expand treatments in order to help control and eliminate parasitic diseases. In working towards the ambitious DIF goal, scaling up treatment to expanded populations and coordination with water, sanitation, and hygiene programs have been prioritized. A partnership with Power of Nutrition, Ethiopia’s nutrition platform, was leveraged to expand NTD treatment to additional at-risk populations, including young children ages 12 to 24 months, children 2 to 5 years, and pregnant women.
The newest fund, the ARISE Fund, will invest in Ethiopia’s efforts to develop resource mobilization strategies and strengthen the leadership and capacity of decision makers who represent communities affected by NTDs. It will also support disease elimination efforts through both innovative and accelerated approaches to implementation; this includes expanding trachoma treatments to include children and increasing the number of TT surgeries to decrease the national backlog.
The Ethiopian FMoH has been a leader in NTD elimination since the launch of its national NTD plan in 2013 and because of the prioritization of NTD programs in its overarching national health strategy. The Ethiopian government has worked closely with national and international partners to reach as many people in need of treatment as possible.
